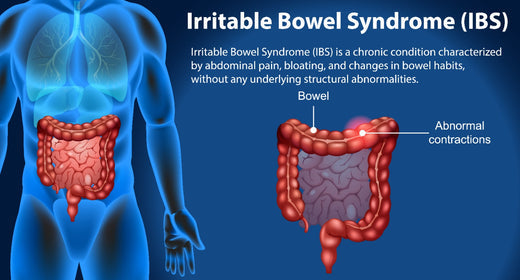
Irritable Bowel Syndrome is described as a chronic gastrointestinal disorder having a spectrum of symptoms such as recurrent abdominal pain, bloating, diarrhoea and constipation. The causative mechanism of IBS is unknown, but it is still believed to be associated with abnormalities in the gut-brain interaction, changes in motility, and inflammation within the gut lining. For many patients, diet plays a key role in the alleviation of symptoms and could eventually serve as a gate pass out of medication. Recognizing the relationship between diet and IBS is essential for appropriate management because it can help a patient with IBS change their dietary strategies and ways of living to improve their quality of life.
Understanding IBS and Its Symptoms
IBS is a functional bowel disorder, meaning that the digestive tract has no visible abnormalities that could explain symptoms. Instead, IBS symptoms are believed to result from abnormal contractions of intestinal muscles, changes in gut microbiota, and increased sensitivity to gut distension and pain.
The main symptoms of IBS include
Abdominal Pain and Cramping: Often described as sharp, stabbing, or a dull ache, that typically gets better after defecation.
Bloating: Continuous distension of the abdomen due to stasis of gas.
Alternating Diarrhea/Constipation: Having loose, fluid stools at times and solid, pellet-like stools others, or one more frequently.
Mucus in Stool: Very common but irritating symptom.
Inadequate Emptying: Feeling that your bowel movements are not satisfactorily completed.
IBS Causes: What Triggers IBS?
The cause of IBS is not found, but several factors are known to trigger the symptoms. Some common IBS causes include the following:
- Problem in the link between gut and brain: The link between gut and brain often gets disturbed in IBS. As a result, the altered brain-gut interaction results in an increased sensitivity to pain and abnormal bowel movements.
- Gastrointestinal infections: Some people suffer from IBS following a severe infection of the gastroenteritis, an illness called post-infectious IBS.
- Stress: Psychological stress and anxiety lead to some symptom manifestations of IBS, thus the strong association between mental states and GI functions.
- Food intolerances: Most people afflicted with IBS are sensitive to specific foodstuffs, and the symptoms will manifest themselves upon consumption of such foodstuffs.
Identifying such triggers and acquiring knowledge of why they induce irritable bowel syndrome is also an integral part of the treatment process. Many find optimal results through the combination of medical therapy, diet changes, and stress reduction measures.
Is IBS passed on through genetics?
Irritable Bowel Syndrome (IBS) is a complex gastrointestinal disorder influenced by multiple factors, including genetics. Studies indicate that IBS tends to run in families, suggesting a hereditary component. Relatives of individuals with IBS are two to three times more likely to develop the condition themselves according to PubMed Central
However, the genetic contribution to IBS is not straightforward. Research has identified over 60 candidate genes potentially associated with IBS, involving pathways like serotonin synthesis and mucosal immune activation.
Despite these findings, no single gene has been pinpointed as a definitive cause. Twin studies further suggest that while there is a genetic predisposition, environmental factors play a significant role in the manifestation of IBS (CGH Journal).
Thus, while genetics may increase susceptibility to IBS, they are just one piece of a larger puzzle that includes environmental influences and lifestyle factors. Ongoing research continues to explore the intricate interplay between these elements to better understand and manage IBS.

Role of Diet in Managing IBS
There are numerous diets that have been proven to help patients alleviate their IBS symptoms. The most studied and applied diet therapy for the treatment of irritable bowel syndrome is the low-FODMAP diet. In this diet, foods containing higher levels of FODMAP are removed from the diet, and they are gradually reintroduced to determine which triggers specific symptoms.
1. Identifying Triggers Foods
Identifying what to avoid and what triggers the symptoms forms the bedrock for managing IBS through diet. Every individual's triggers will vary, but common triggers include:
FODMAPs: These are short-chain carbohydrates and sugars that the body fails to absorb in the small intestine. Bacteria in the colon ferment them, causing gas and bloating. Onions, garlic, beans, lentils, dairy products, certain fruits, and sorbitol are common examples of FODMAPs.
Gluten: In some cases, gluten, a protein found in wheat, barley, and rye, exacerbates symptoms.
Fatty Foods: High-fat foods will tend to slow down digestion, exacerbating symptoms of diarrhea and abdominal pain.
Caffeine: Can irritate the gut and cause symptoms to worsen.
2. The Low-FODMAP Diet
The low-FODMAP diet is perhaps the most frequently recommended diet for IBS symptom management. It requires one to temporarily cut out high FODMAP foods and reintroduce these systematically to pinpoint individual offenders. This diet has been proved to greatly benefit IBS symptoms in most people.
The process mainly includes the following steps:
Elimination Phase: Restrict FODMAPs to know their effects on symptoms. This phase might take 4-6 weeks.
Reintroduction Phase: Re-introduce FODMAP one at a time to check out which are causing some reactions.
Personalization Phase: Tailoring the diet to contain only the harmless FODMAPs thereby allowing the patient to incorporate the diet without discomfort.
3. High-Fiber Diet
Adding fiber to the diet also plays an important role in the treatment of IBS. A high fiber diet may help maintain the movement of the bowel and alleviate constipation. Soluble fibers like oats, carrots, and barley are highly effective since they can absorb water and make the stool soft; this facilitates easy passage through the bowels. On the other hand, insoluble fibers present in wheat bran sometimes make symptoms worse for those who have IBS.
4. Probiotics and Prebiotics
Live helpful bacteria for digestive health, probiotics can alleviate IBS by reducing the amount of gas in the system. Research further indicates that the use of certain probiotics such as Lactobacillus and Bifidobacterium can result in the minimization of bloating and effective bowel functions. Prebiotics feed good bacteria and enhance health. They increase the volume of beneficial microorganisms in the intestine. These could be bananas, onions, garlic, or asparagus.
5. Elimination diets and food sensitivities
The elimination diet may also be taken as other than the low-FODMAP diet. It's most indicated in the conditions when food sensitivities are thought to be the probable causative factor of IBS-like symptoms. These include lactose intolerance or fructose malabsorption.An elimination diet will have the suspected trigger foods removed and then reintroduced singly to determine which foods bring back symptoms.
Other IBS-Friendly Diet Strategies
In addition to the Low-FODMAP diet, there are other dietary recommendations that could help regulate the symptoms of IBS:
- Eat in Smaller, More Frequent Meals: While eating in large amounts at once could overstimulate the gut, causing bloating and discomfort, it is much easier for the system to digest small, frequent meals.
- Drink Ample Fluids: Maintenance of the body's hydration by drinking plenty of water would maintain a proper bowel movement and avoid cases of constipation.
- Include Soluble Fiber: Oats, flaxseeds, and carrots are a few which consist of high percentages of soluble fiber and will help promote bowel movements without causing irritation.
Conditions similar to IBS
Several conditions share symptoms with Irritable Bowel Syndrome (IBS), making accurate diagnosis essential. Here are some conditions that can mimic IBS:
Celiac Disease
An autoimmune disorder where ingestion of gluten leads to damage in the small intestine, causing symptoms like diarrhea, bloating, and abdominal pain. Unlike IBS, celiac disease can result in nutrient deficiencies and requires a gluten-free diet for management.
Lactose Intolerance
The inability to digest lactose, a sugar found in milk and dairy products, leading to bloating, diarrhea, and gas. Symptoms typically occur within two hours of consuming dairy and can be managed by avoiding lactose-containing foods.
Diverticulitis
An inflammation or infection of small pouches (diverticula) that can form in the walls of the colon, causing symptoms like abdominal pain, fever, and changes in bowel habits. Unlike IBS, diverticulitis may require medical treatment or surgery.
Inflammatory Bowel Disease (IBD)
Includes Crohn's disease and ulcerative colitis, characterized by chronic inflammation of the gastrointestinal tract. Symptoms overlap with IBS but often include weight loss, blood in stools, and fatigue. IBD requires medical intervention and monitoring.
Endometriosis
A condition where tissue similar to the uterine lining grows outside the uterus, causing severe abdominal pain, bloating, and changes in bowel habits. It predominantly affects women and may require surgical intervention.
Given the overlap in symptoms, it's crucial to consult a healthcare professional for proper evaluation and diagnosis.
Medical Treatment of IBS
Even though diet plays a crucial role in managing IBS, some patients may require some medical interventions. These are complementary parts of the treatment of irritable bowel syndrome and include:
- Antispasmodic drugs: These mediate the relaxation of the muscles within the gut, hence reducing cramping and pain.
- Laxatives or anti-diarrheal medicines: This depends on the type of IBS: constipation or diarrhea.
- Probiotics: These good bacteria may have positive effects on the gut, as well as alleviate IBS symptomatology, though more research is needed to confirm the efficacy of probiotics.
- Psychological therapies: Stress and anxiety can trigger IBS symptoms; therefore, treatments such as CBT and mindfulness training may help by modulating the brain-gut interface, thus alleviating symptoms.
Take a gut health test for IBS today
Lifestyle Interventions for IBS Management
Lifestyle changes are integral in proper management of IBS. Dietary changes are at the foundation of treatment; there's a reduction of triggering foods and a low FODMAP diet for most patients. In addition to these diet changes, many will also find relaxation techniques beneficial in managing their stress; with yoga, mindfulness meditation, or breathing exercises being just some of the useful ways that help in controlling it in most people.
Practices can help reduce stress levels by improving gastrointestinal function, providing adequate gut motility, as well as reducing symptoms caused by abdominal pain and bloating. Regular physical activities and sufficient sleep are added elements of an effective plan to manage IBS effectively. These lifestyle interventions prevent symptoms but also enhance good time and quality of life through improved well-being for sufferers with IBS.
Myths and Misconceptions About Diet and IBS
Despite the growing insight into diet in managing IBS, many myths and myths still prevail:
"All Fiber is Bad for IBS": Although fiber intake may exacerbate symptoms by some types, soluble fibers are beneficial in the treatment of IBS and are acceptable in the diet of those who tolerate them.
"Probiotics are the Cure for IBS": These may be helpful in symptom alleviation but are definitely no cure and must be used in relation to a broader management scheme.
"Avoiding all Dairy is Necessary for IBS": Not everyone with IBS needs to avoid dairy. Most can tolerate lactose-free dairy products.
"Low-FODMAP Diet Is the Only Way to Manage IBS": Although very effective for many, the low-FODMAP diet is definitely not the only option. Instead, it should be made according to individual needs and symptoms.
Conclusion
IBS may dramatically affect a person's quality of life, but dietetic intervention is an emerging strategy to manage this condition. Avoiding trigger foods, a low-FODMAP diet, probiotics, and prebiotics have been demonstrated to effectively decrease symptoms and improve gut health.
Lifestyle modifications include regular exercise and stress management, among others, in the management of IBS. Close teamwork between an individual and their health care provider is vital for working out a personal, well-designed plan to treat one's unique triggers and symptoms.
Understanding the causes of IBS and which foods to avoid with IBS can then reclaim control over one's digestive health and implement effective strategies for long-term relief. For more personalized advice on how to deal with IBS by means of diet plans and stress management, check out Sova.Health. Improve your digestive health and well-being today with expert guidance.